Evidence Based Practice in Long Term Care Facilities
Value-Based Care at Hopkins
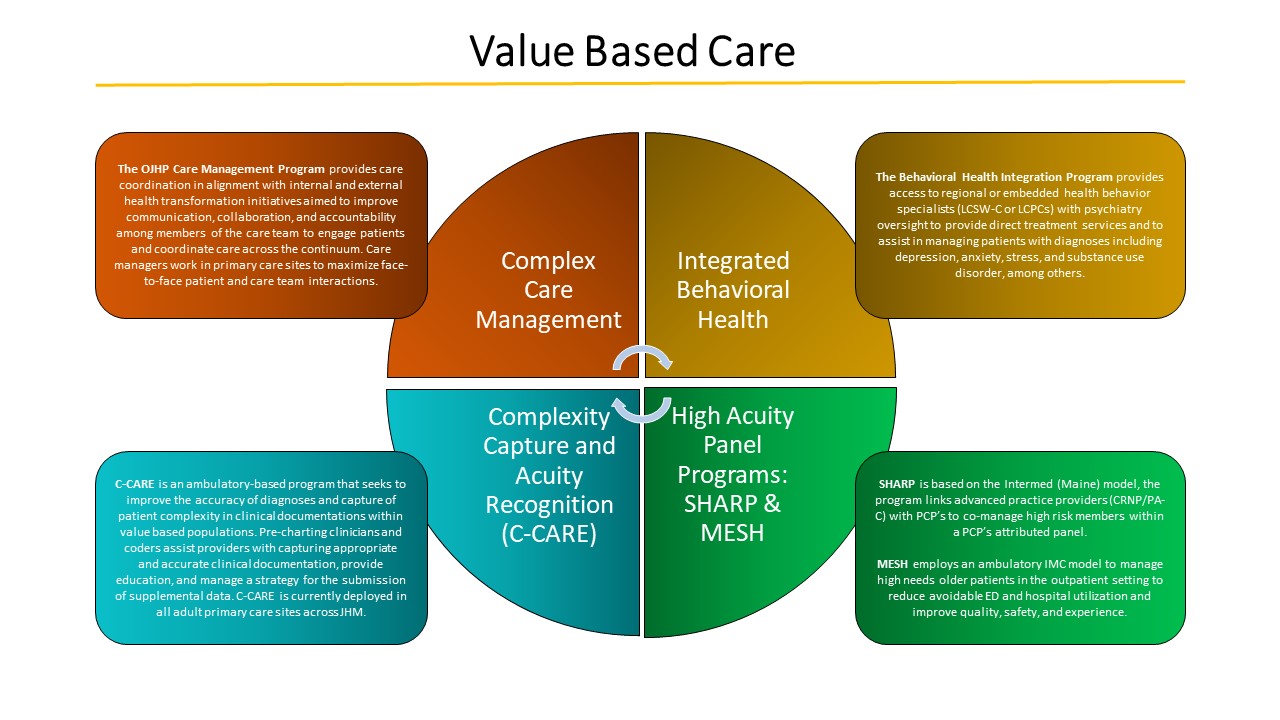
We are delivering more healthcare within a "value-based" framework, with goals of improving the patient's experience of care, improving the health of populations, and reducing per capita costs. The Office of Johns Hopkins Physicians administers a set of Value-Based Care (VBC) resources to improve outcomes across all of our patients.
Medically complex patients, and patients with complex social needs, require special attention. OJHP is developing a suite of services to address the needs of these unique individuals
Clinical Topics:
- SHARP: Small High Acuity Risk Panel
- MESH: Multidisciplinary Empowerment for Sustained Health
- PAPC: Priority Access Primary Care
Care Management Resources:
- Complex Care Management
- Integrated Behavioral Health
Value-Based Care Education
- Complexity Capture and Acuity Recognition (C-CARE)
- Overview of Value-Based Healthcare concepts (under construction)
Complex Care Management
The OJHP Care Management program is a care coordination model in alignment with internal and external health transformation initiatives aimed to improve communication, collaboration, and accountability among members of the care team to engage patients and coordinate care across the continuum. Care managers are embedded at primary care sites to maximize face-to-face patient and care team interactions for high-risk and rising risk populations who could benefit from care management services.
For more information:
Email Dawn Sagliani
Integrated Behavioral Health
The Behavioral Health Integration Program provides access to regional or embedded health behavior specialists (LCSW-C or LCPCs) with psychiatry oversight to provide direct treatment services and to assist in managing patients with diagnoses including depression, anxiety, stress, and substance use disorder, among others. Patients are identified for enrollment through both direct referrals and patient risk lists generated through the Tableau Harmonized Medicare & Medicare Advantage Dashboard. Health Behavior Specialists (HBS) are integrated within primary care practices.
Small High Acuity/Risk Panel (SHARP)
Based on the Intermed (Maine) model, the SHARP Program is an evidence-based advanced practice provider (CRNP/PA-C) led high risk patient management model that integrates into existing primary care practices in which the SHARP-designated provider co-manages high risk members within a PCP's attributed panel. The overall goal of SHARP is to improve outcomes and reduce unnecessary costs of care for high risk patients through an innovative, interdisciplinary approach, creating a dynamic partnership with one's care team. SHARP is currently available at the JHCP practices at White Marsh, EBMC, Westminster and Hagerstown and coming to the Odenton, Remington, and Greater Dundalk practices in Q1/Q2 of FY2021.
For more information:
Email Mike Albert, MD
Complexity Capture and Acuity Recognition (C-CARE)
C-CARE is an ambulatory-based program that seeks to improve the accuracy of diagnoses and capture of patient complexity in clinical documentations within value based populations. This is achieved through a combination of employing pre-charting clinicians and coders to assist providers with capturing appropriate and accurate clinical documentation, providing tailored provider education, and managing a strategy for the submission of supplemental data. C-CARE is currently deployed in most primary care sites.
For more information:
Email Maura McGuire, MD
Multidisciplinary Empowerment for Sustained Health (MESH)
MESH employs an ambulatory IMC model to manage high needs patients in the outpatient setting with the objective to reduce potentially avoidable ED and hospital utilization while maintaining and improving patient quality, safety, and experience. Patients are managed through a high touch, team base approached that includes customized care plans, protocolized touchpoints, increased patient contact, care team huddling and coordination, and a combination of clinic, home, and group encounters until the patient is deemed stable to return to standard primary care. Based in the Johns Hopkins Bayview Medical Center primary care sites.
For more information:
Email Heather Agee, MD
Risk Adjustment Education
We are delivering more healthcare within a "value-based" framework, with goals of improving the patient's experience of care, improving the health of populations, and reducing per capita costs. The Office of Johns Hopkins Physicians administers a set of Value-Based Care (VBC) resources to improve outcomes across all of our patients.
Evidence Based Practice in Long Term Care Facilities
Source: https://www.hopkinsmedicine.org/office-of-johns-hopkins-physicians/education-training/value.html
0 Response to "Evidence Based Practice in Long Term Care Facilities"
Post a Comment